 |
CYP3A4 DDIdB A database of CYP3A4-mediated drug interaction on anti-HIV and anti-TB drugs |
 |
|
Cytochrome P450
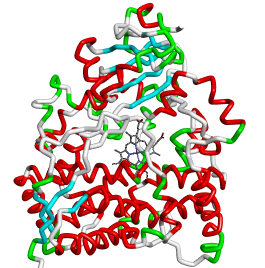
Cytochrome P450 enzymes are large and diverse superfamily of heme containing enzymes (hemoproteins) that catalyze the oxidative metabolism of wide variety of endogenous compounds, including fatty acids, steroids, prostaglandins, biogenic amines and pheromones, as well as for exogenous compounds such as drugs, pollutants, environmental compounds, plant metabolites and food additives (for review see Wrighton and Stevens, 1992). These enzymes show maximum absorption at the wavelength of 450 nm and hence named as P450, where P stands for pigment (Klingenberg, 1958; Omura and Sato, 1964). The catalytic mechanism is common to all CYP proteins, in which one oxygen atom of molecular oxygen (O2) is transferred into substrate molecule and another oxygen atom is reduced into water molecule (Guengerich, 1996; Ortiz de Montellano, 1999; Vaz, 2003; for review see Guengerich, 2001). This catalytic cycle requires input of two reducing equivalents from the cofactor NADPH (Guengerich, 1996; for review see Lewis and Pratt, 1998). The various metabolic reactions catalyzed by cytochrome P450 family include aromatic oxidation, aliphatic oxidation, epoxidation, dealkylation, oxidative deamination, N-hydroxylation, N-oxidation, sulfoxidation and desulfuration (Lewis, 1996). Cytochrome P450 enzymes have been identified in almost all organisms, including animals, insects, plants, fungi, protists, bacteria, archaea and viruses (Nelson, 2009; for review see Danielson, 2002). CYP enzymes are classified into families and subfamilies based on their amino acid sequence identity. The CYP isoenzymes having at least 40% identity are classified into different families, and those isoenzymes in the family having at least 55% identity are further grouped into subfamilies. The nomenclature of P450 enzymes describe CYP denoting superfamily, followed by an Arabic number indicating family, a capital letter designating subfamily and again a number indicating individual gene within subfamily (Nelson, 1996, 2006; Martikainen, 2012). Currently a total of 11,294 individual genes, 977 families and 2,519 subfamilies have been identified from various species (Nelson, 2009). Fifty-seven individual genes of CYP enzymes were reported to exist in human genome and it is classified into eighteen families and forty-three subfamilies (http://drnelson.uthsc.edu/human.P450.table.html) (Lewis, 2004; Nelson, 2004). Of these, CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP2E1 and CYP3A4 are the major isoforms involved in 90% of drug metabolism in humans (for review see Daly, 2004). Among CYP enzymes, CYP3A4 (CYP3 family) is contributing to metabolism of more than 50% of all clinically used drugs (for review see Wrighton et al., 2000). Thus, it is not surprising that Drug-drug interactions more often occur due to the inhibition or induction of CYP3A4 enzyme by concomitantly administered drugs. Hence, a better understanding of CYP3A4-drug interaction mechanisms would be of great importance to any new drug discovery effort. Cytochrome P450 3A4 Cytochrome P450 3A4 (CYP3A4) is one of the most abundant CYP enzymes in liver (Shimada et al., 1994) and present in small intestine to a lesser extent (Zhang et al., 1999). This enzyme is localized in endoplasmic reticulum of the cells. It catalyzes the metabolic reactions of wide range of bulky substrate molecules, such as bromocriptine, cyclosporine, taxanes and erythromycin (Ekroos and Sj?gren, 2006; for reviews see Li et al., 1995; Rendic, 2002), and biosynthesis of endogenous molecules such as steroids, fatty acids and other lipids. Clinically important drugs have been identified as substrates, inhibitors and/or inducers of the CYP3A4 enzyme for metabolic oxidation (Flockhart, 2007). Disposition, efficacy and toxicity of known CYP3A4 substrate is the measure to predict the drugs activity as substrate, an inhibitor and/or an inducer of the CYP3A4 enzyme, when co-administered (for review see Zhou, 2008). However, some of the drugs may have all the three activities together, e.g., anti-HIV drugs, efavirenz, ritonavir and nelfinavir (for review see Piscitelli and Gallicano, 2001). Some of the clinically relevant CYP3A4 substrates include macrolide antibiotics (clarithromycin and erythromycin), benzodiazepines (alprazolam, midazolam, and triazolam), immune modulators (cyclosporine and tacrolimus), HIV antivirals (indinavir, nelfinavir, and saquinavir), antihistamines (astemizole, chlorpheniramine and terfenadine), calcium channel blockers (amlodipine, felodipine and nisoldipine) and HMG-CoA reductase inhibitors (atorvastatin, cerivastatin and lovastatin) (Flockhart, 2007). CYP3A4 inhibitors reduce the activity of CYP3A4 enzyme and consequently increase the concentration of CYP3A4 substrate drug in the plasma. Drugs such as ketoconazole, ritonavir, delavirdine and imatinib are some of the examples of potential CYP3A4 inhibitors. CYP3A4 inducers interact with xenobiotic-nuclear receptor, particularily in pregnane X receptor (PXR) or constitutive androstane receptor (CAR) that induce the expression of CYP3A4 and consequently increases its metabolic activity (for review see Tompkins and Wallace, 2007). Examples of CYP3A4 inducers include barbiturates, dexamethasone, glucocorticoids, phenytoin and rifampin (Flockhart, 2007). References
|
|
|