 |
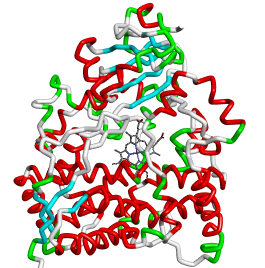
CYP3A4 DDIdB A database of CYP3A4-mediated drug interaction on anti-HIV and anti-TB drugs |
 |
|
Drug-drug interactions
Drug-drug interactions occur when two or more drugs of the same metabolizing enzyme are co-administered, in which one drug competes with another drug for binding to the same active site of the enzyme for oxidative metabolism (for reviews see Tanaka, 1998; Ogu and Maxa, 2000). These interactions could lead to altered rates of metabolism of the competing drugs in the plasma, resulting in increased drug toxicity, decreased therapeutic efficacy and adverse drug reactions (ADR). The Drug-drug interactions in cytochrome P450 primarily occur either through its inhibition or induction effect by the drugs, towards metabolizing the cytochrome P450 substrates. The inhibition of drug metabolism occurs when co-administered with other CYP substrates or inhibitors, whereas drug induction occurs via binding to the xenobiotics nuclear receptor, in particular PXR that induces the CYP enzyme expression (for reviews see Ogu and Maxa, 2000). Hence, it is important to identify the type of cytochrome P450 that metabolizes a specific drug, so that the occurrence of Drug-drug interactions could be managed by avoiding the use of drugs that interact with same drug metabolizing enzyme during co-administration. Of the available cytochrome P450 isozymes, CYP3A4 plays important role in the oxidative metabolism of majority of currently marketed drugs and involves in significant Drug-drug interactions (Flockhart, 2007). Drug-drug interactions usually take place in the combination therapy, in which two or more different classes of drugs are co-administered to target diseases. The most significant examples of diseases, in which Drug-drug interactions occur, include acquired immunodeficiency syndrome (AIDS), tuberculosis, cancer, leprosy and malaria (Marechal et al., 2006). Drug-drug interactions in HIV treatment Human immunodeficiency virus, which causes AIDS in the humans, is one of the important targets for clinical research. The current antiretroviral therapy (ART) for HIV infection, known as highly active antiretroviral therapy (HAART), consists of concurrent administration of three or more different classes of antiretroviral drugs to suppress the viral replication and to prevent the occurrence of drug resistance. The primary goals of such a combination of antiretroviral drugs are (1) to reduce HIV associated mortality and morbidity, (2) to improve the function of immune system, (3) to suppress the progression of viral load in the plasma and (4) to prevent HIV transmission. (for review see Maenza and Flexner, 1998; Panel on Antiretroviral Guidelines for Adults and Adolescents, Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents, Department of Health and Human Services). Various classes of antiretroviral drugs for HIV treatment include nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), fusion inhibitors, CCR5 antagonists and integrase inhibitors (Drugs@FDA). The first two classes of drugs, NRTIs and NNRTIs, inhibit the replication cycle of the viral genome. PIs inhibit function of viral protease enzyme, which is required for the activation of the nascent polyproteins into fully mature functional protein through proteolytic cleavage (Dickson et al., 1982). The fusion and CCR5 inhibitors block the entry of HIV virus into their target host cells by binding to gp41 and CCR5 receptors respectively (Flexner, 2007). Finally, integrase inhibitor targets HIV integrase enzyme, which integrates HIV genetic material into the host cell genome. Inspite of significant control in progression of HIV through combination therapies of HAART, it complicates the HIV treatments in choosing the right choice of drugs from the available different class of antiretroviral drugs. The Drug-drug interactions are predominantly unavoidable in HAART due to the concurrent co-administrations of antiretroviral drugs to the HIV infected patients. The three classes of antiretroviral drugs, such as PIs, NNRTIs and entry inhibitors, are all metabolized by cytochrome P450 enzymes, particularly CYP3A4. In addition, most of these drugs also act as inhibitors of this enzyme. Hence, the co-administration of these three classes of antiretroviral drugs may lead to competitive binding towards the active site of CYP3A4 enzyme, resulting in altered metabolism and increased toxicity of competing drugs in the plasma (Tanaka, 1998; Ogu and Maxa, 2000; Gonzalez and Tukey, 2005). Some of the common adverse effects of these antiretroviral drugs include liver toxicity, gastrointestinal intolerance, esophageal candidiasis, neuropsychiatric symptoms, and glucose and lipid abnormalities. Thus, a better understanding of Drug-drug interactions among PIs, NNRTIs and entry inhibitors governed by CYP3A4 could help us in choosing the right choice of drugs to be used in combination therapy. Drug-drug interactions in the treatment of HIV-related tuberculosis Tuberculosis (TB) is a common opportunistic infection among people infected with HIV. The World Health Organization (WHO) estimated that 1.1 million new HIV-related TB cases were found globally in the year 2011. Worldwide, thirty-four million people are infected with HIV, of which at least one-third of the people are also infected with tuberculosis. One-fourth of deaths in HIV infected people are due to the incidence of tuberculosis. Around 430,000 people died of HIV-related tuberculosis globally in 2011 as per the WHO’s TB/HIV facts 2012-2013 The complications associated with treatment of HIV/TB co-infection is the occurrence of Drug-drug interactions between anti-tuberculosis drugs (rifampin, rifapentine, rifabutin, isoniazid and pyrazinamide) and antiretroviral drugs (PIs and NNRTIs). These interactions occur through induction or inhibition of CYP3A4 enzyme, resulting in sub-therapeutic level or increased toxicity of co-administered drugs (for reviews see Burman et al., 1999; Burman and Jones, 2001). References
|
|
|